 Dr Rishma Pai
Dr Rishma Pai
MD, FRCOG, DNB DGO FCPS FICOG Consultant Gynaecologist and IVF Expert at Lilavati and Jaslok & Hinduja Healthcare (Khar)
Hospitals Mumbai,
President – Federation of Obstetric
and Gynaecological Societies of
India 2017.
President (Elect) of the Indian
Society of Assisted Reproduction
What couples need to know about getting pregnant.
What is Infertility?
Approximately 80% to 85% of couples who are trying to become pregnant will successfully conceive within a year. Thus, we commonly define infertility as the inability to achieve a pregnancy within 12 months of unprotected intercourse.
Fertility potential declines significantly as a woman ages, hence couples are encouraged to seek evaluation for infertility after 6 months of no contraception if the woman is older than age 35.
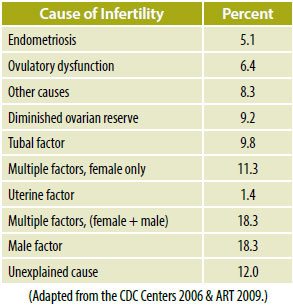
What are typical causes of infertility?
The causes of infertility are wide ranging. They can be equally divided between the male and female partners in a couple.
What Tests Will the couple have to Undergo as Part of a Fertility Evaluation?
Evaluation of Female Partner
1] Assessment of ovulation:
(The growth and release of egg from the ovary)
Tests of ovulation:
- Basal body temperature: Based on progesterone rise after ovulation, reflecting rise in basal body temperature by 0.50C.
- LH surge detection: Identifies mid cycle LH surge which precedes ovulation by 1-2 days. Urine testing kits are available for home use.
- Transvaginal scan: TVS helps monitoring egg growth and confirming rupture
- Serum progesterone: Blood test on day 21 of menses >10ng/mL suggests ovulation
Transvaginal ultrasound allows the physician to assess the appearance of the uterus and the ovaries. During this examination, the physician may discover uterine abnormalities such as fibroids (benign growths of the muscle of the uterus) or uterine polyps (benign growths of the lining of the uterus) also presence of ovarian cysts.
2] Ovarian reserve tests:
 Ovarian reserve is a function of number and quality of oocytes. Women with decreased ovarian reserve (DOR) may have regular or scanty menses and response to stimulation is decreased when compared to other woman of the same age.
Ovarian reserve is a function of number and quality of oocytes. Women with decreased ovarian reserve (DOR) may have regular or scanty menses and response to stimulation is decreased when compared to other woman of the same age.
- Day 2-4 values of FSH >10 IU/L predicts poor response
- Anti-mullerian Hormone : AMH is a simple blood test which tells you about the number of small eggs in the ovary. Serum values of less than 1 ng/ml are associated with poor ovarian response
- Antral follicle count : measured by a transvaginal sonography and defined as total number of small eggs in the ovaries. Less than 3 -4 eggs per ovary is a poor responder.
3] Tubal testing:
Tubal testing can be done by hysterosalpingography which is a X ray of the womb done on day 6 of menses.
Endoscopy, laparoscopy or key hole surgery is the other best technique for checking the tubes alongwith any other problems in the uterus or ovaries.
EVALUATION OF MALE PARTNER:
- Semen Analysis:
Routine testing of the male partner of an infertile couple includes a basic semen analysis evaluating the volume of semen, the concentration of sperm (sperm count), the percentage of moving sperm (sperm motility), and the percentage of normally shaped sperm (sperm morphology). Sometimes there may be a need to do hormone evaluation, genetic tests or a biopsy of the testes if no sperms are there in the semen sample
- Complete hormonal profile: In severely altered semen parameters, hormonal assays like FSH, testosterone, and TSH and prolactin may be done.
 Dr Hrishikesh Pai
Dr Hrishikesh Pai
MD, FCPS FICOG MSc USA
Consultant Gynaecologist and
IVF Specialist, Bloom IVF Centre,
Lilavati Hospital Mumbai, Fortis
Hospitals at New Delhi / Gurgaon /
Noida / Faridabad / Mohali & Vashi, D Y Patil Hospital, Navi Mumbai
Secretary General of the
Federation of Obstetric and
Gynaecological Societies of India.
What is Laparoscopy?
A laparoscopy or key hole surgery is usually performed under general anaesthesia.
During a laparoscopy, the physician inserts a small fiberoptic telescope into the abdominal cavity through an incision made in the patient’s umbilical area (belly button). Using the laparoscope, a gynecologic surgeon can inspect the uterus, fallopian tubes, and ovaries. During a laparoscopy, the physician typically introduces a blue dye into the uterine cavity while directly visualizing the fallopian tubes. If abnormal ovarian cysts such as endometriomas or fibroids are present, then the physician may remove them during the course of the laparoscopy.
What is Hysteroscopy
A hysteroscopy is a simple surgical procedure that is performed either to diagnose or to treat a problem within the uterine cavity. During hysteroscopy, the physician inserts a small fiber-optic telescope through the cervix and into the uterus. Liquid can be used to distend the uterus and allow the physician to directly visualize the uterine cavity. The physician may also introduce small instruments into the uterus to cut scar tissue or remove polyps or fibroids.
Hysterosalpingogram (HSG). In this a radiopaque fluid is introduced into the uterine cavity under fluoroscopy (X ray), the dye is observed as it fills the uterine cavity and then passes out into the fallopian tubes and ultimately spills out of the ends of the tubes and into the pelvis. The HSG can be used to diagnose polyps and fibroids. This imaging procedure also provides information on the status of the fallopian tubes. However, this is a painful procedure as it is usually done without anaesthesia.
How does an Infertility specialist determine a Plan of Therapy?
A particular course of treatment is recommended only after performing a complete fertility evaluation that usually includes a pelvic ultrasound, an assessment of tubal patency a semen analysis, and a variety of hormonal blood tests.
The treatment plan for any couple is unique to them. If testing has demonstrated a clear problem, such as blocked fallopian tubes or a markedly abnormal sperm count, then in vitro fertilization (IVF) may be recommended as the only reasonable alternative. However, most couples are not sterile but merely subfertile, so they may be offered a range of therapeutic options from simple planned intercourse —to the use of semen insemination with or without fertility drugs, to IVF or intracytoplasmic sperm injection (ICSI).
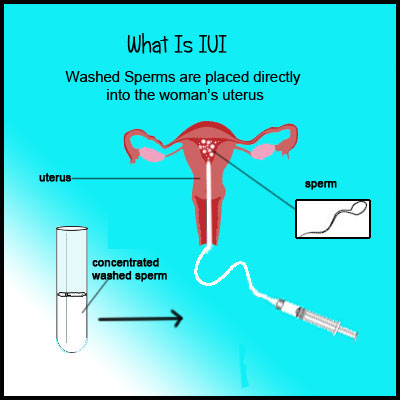
What is Intrauterine Insemination (IUI)?
This technique is for women with open tubes and where the sperm count is nearly normal. When performing an IUI, the sperm must first be washed and prepared prior to placement inside the uterus. Washing the sperm removes the prostaglandins that cause the violent uterine contractions. Washing also eliminates substances that might lower the sperm quality and activates the sperm, thereby leading to improved sperm motility.

The actual IUI is a painless, simple, in-office procedure. It usually takes just a minute to perform.
What is IVF and how is it performed?
In vitro fertilization (IVF) was first successfully performed in Oldham, England, in 1978, resulting in the birth of Louise Brown.
IVF literally means “the fertilization of eggs with sperm in glass,” which translates to fertilization outside of the body in the laboratory.
Phase 1: Ovarian Stimulation
A woman’s ovaries contain thousands of fluid-filled sacs called follicles. Inside each follicle is an egg (or ovum). In a normal reproductive cycle, only a single follicle (and egg) reaches maturity. For IVF, injections are given to increase the number of eggs which grow. Usually 5 – 10 eggs are made to grow and monitored with regular sonography. It takes about 11 days for the eggs to get ready to remove, when the size reaches 17 – 20 mm.
Phase 2: Oocyte Retrieval
The egg collection is performed under intravenous sedation or general anaesthesia using a vaginal ultrasound probe with a special needle guide adapter. The needle passes through the side of the vagina into the ovary, and the follicles are easily aspirated. The fluid containing the eggs is then inspected by the embryologist using a microscope. In typical IVF both the eggs and the sperm are then placed together in small plastic dishes containing media and incubated for the next 3 to 5 days. If there is a significant male factor or any other indication, then ICSI is performed several hours after the egg collection.
Phase 3: Embryo Culture
In general, about 70% of the mature eggs will fertilize in the laboratory. Unfortunately, some attrition occurs at each point in an IVF cycle so the total number of healthy embryos is often much less than the original number of follicles or eggs. Three days after the egg collection procedure, the embryos selected for embryo transfer will be identified. Allowing the embryos to grow for an additional 2–3 days in the laboratory culture (Blastocyst) may allow for enhanced embryo selection as some excellent appearing day 3 embryos will fail to continue to grow.
Phase 4: Embryo Transfer
Embryo transfer is one of the most important aspects of an IVF cycle. During this phase, the embryos are transferred into the uterus by a thin tube under sonograppy control. No anaesthesia is usually required for an embryo transfer and this step usually takes only 1–2 minutes to complete.
Phase 5: Post-Transfer and Pregnancy
During the 2 weeks after the embryo transfer, patients take supplemental progesterone (shots and/or suppositories) and estrogen.
Two weeks after the transfer, the woman typically undergoes a blood test called serum beta Hcg to confirm if there is a pregnancy or not.
 Dr. Dhanashri Natu
Dr. Dhanashri Natu
MS DNB OBGYN
FNB Fellow in Reproductive
Medicine
How successful is IVF?
The success of IVF cycle depends on:
- Patient’s age
- Cause of infertility
- Duration of infertility (Best prognosis if <5yrs)
- Experience/expertise of the clinic
- Number of embryos transferred
- Type of IVF performed: Stimulated vs. Natural Cycle IVF
What is ICSI and how does it differ from IVF?
Intracytoplasmic sperm injection (ICSI), in that each egg is individually injected with a single sperm using a tiny needle under microscopic guidance. The resulting embryo is then cultured in the lab.
ICSI is simply a method to ensure that the egg is fertilized in cases where IVF fails or when the sperm count is very low.
Who needs ICSI ?
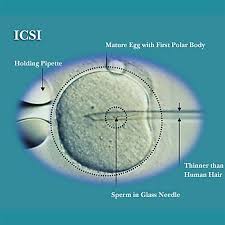
The most common indication for ICSI is male factor infertility associated with an abnormal semen analysis. Therefore, men whose sperm count, motility or morphology is poor are appropriate candidates for ICSI in order to ensure fertilization of the egg.
Another common indication for ICSI is unexplained infertility. In these couples, neither the man nor the woman has any apparent fertility-related problems. Their diagnostic evaluation is entirely normal, yet infertility exists. In such couples, by using ICSI, the eggs are “forced” to fertilize, and the pregnancy rates are usually high. Fertilization rates with ICSI are usually 60%–80% depending upon egg and sperm factors.
What Is embryo freezing ?
Embryos can be cryopreserved by freezing them in liquid nitrogen. Through a series of carefully orchestrated steps, the embryos are ultimately frozen at a temperature of –196 C, leaving them in a state of suspended animation in which they can remain for many years. The pregnancy rates associated with replacing frozen embryos depend on the age of the patient and the quality of the embryos at the time of cryopreservation. With the new technique of vitrification or rapid freezing, the pregnancy rates after embryo freezing are excellent.
Can I freeze my eggs now so that I can use them in the future?
Recent advances in egg (oocyte) and embryo cryopreservation have radically changed our approach. Egg freezing is now a viable option for fertility preservation. With the use of “vitrification” (ultra-fast cooling technology), egg survival, fertilization and pregnancy rates have vastly improved. Egg freezing is no longer just a “backup” experimental procedure, but rather it represents an advanced reproductive technology for women wishing to preserve their fertility.
Reasons for egg freezing:
- Can be offered in woman who want to delay childbirth
- In patients who are at risk of premature ovarian failure like patients on chemotharapy, genetic conditions, ovarian surgery. Egg cryopreservation involves the same steps in a stimulated IVF treatment. The patient takes gonadotropin injections for about 10 days to induce the development of multiple follicles. The eggs are then collected using transvaginal sonography under general anaesthesia and immediately cryopreserved using “vitrification.” Theoretically, the eggs can be stored indefinitely for later fertilization and embryo transfer.
What are the options in women who are older or have no eggs in their ovaries?
After the age of 30, fertility begins to decline, markedly so after the age of 35. By age 40, most women will experience infertility as the ovarian reserve is depleted.
When a woman’s response to fertility medication is poor, or when she has failed to conceive with previous attempts at IVF or other treatments, or when she has diminished ovarian reserve, then IVF using donor eggs is an excellent option. By using donated eggs from a woman in her twenties, the infertile patient essentially restores her fertility potential to that of the age of her egg donor. Similarly, the miscarriage rate drops from more than 50% for patients older than age 40 to 10% to 12% with the use of donor eggs. Egg donation has been used extensively in patients who are perimenopausal or even menopausal.
What is a surrogacy and when should you consider using one?
A gestational carrier or surrogate is a woman who has agreed to carry a pregnancy for another woman/couple because the latter has been determined to have medical issues that make a successful pregnancy extremely unlikely or dangerous. A surrogate gives no genetic contribution to the baby that only carries the embryo from the genetic parent.
Many medical conditions necessitate the use of a surrogate, including the absence of a uterus in the would-be mother, either because of a congenital (at birth) condition or when a disease necessitated its surgical removal. Surrogacy may also be the best option when a woman has a systemic disease that may affect either her own or her baby’s health, such as advanced heart disease, severe diabetes, or multiple sclerosis. Likewise, a woman with a history of poor pregnancy outcome including repetitive pregnancy losses, preterm labour, incompetent cervix, or severe preeclampsia may be a good candidate for IVF using a surrogate mother.
What are the options for men with zero sperm count.
In these men, a serum FSH level is done. If the hormone test is normal, sperm can be obtained from the testes by a simple needle biopsy. The techniques of PESA (Percutaneous epididymal sperm aspiration) and TESA (Testicular sperm aspiration) gives good results to obtain sperms. This is followed by ICSI and many such men can become fathers.
What happens in cases with advanced sperm retrieval techniques when no sperm is obtained?
Couples who desire a child but in whom the male partner has a very low sperm count (oligospermia) or no sperm at all (azoospermia) often consider using sperm donation and Artificial Insemination (Artificial Insemination). The donated sperm is obtained from the donor, tested, and quarantined for at least 6 months at the sperm bank.
What are the new techniques available in advanced fertility centres ?
In top of the line clinics highly progressive techniques are being used which are
- IMSI: IMSI technique give excellent results for men with very poor sperm parameters and for repeated IVF failures or repeated miscarriages.
- Embryoscope: The Embryoscope™ is an advanced non- touch incubator that maintains the necessary physiological conditions required by a living embryo while they are in the IVF laboratory. It has an incorporated time lapse system that has a camera that continuously captures images and records them as a video of the embryonic development. This system allows the embryologist to monitor embryo cell divisions while the embryos are still in the incubator and we can carry out a study of the development of the embryos. This can help choose the best embryos among all the embryos of the patient

- Assisted hatching: Here the outer cover of the egg can be thinned or cut open before putting the embryos into the womb. This helps implantation and pregnancy rates.
- PGD and PGS: A tiny biopsy of the embryo (1 – 2 cells) is taken and genetically analysed rapidly. Only normal embryos are selected for transferring into the womb. This is particular useful for families with a previous abnormal child or repeated miscarriages.
Today most couples with difficulty in becoming parents, can be helped by advanced fertility treatments. The important thing is to seek help early and from the right well experienced and trained fertility specialists.























