
 Importance of Science and Evidence as being Central to Public Health policy
Importance of Science and Evidence as being Central to Public Health policy
Dr Soumya Swaminathan,
Deputy Director General, Programmes, WHO
Soumya Swaminathan, an Indian Paediatrician and Clinical Scientist holds M.B.B.S. from Armed Forces Medical College and M.D. from AIIMS, Delhi, along with a Diplomate of National Board from National Board of Examinations. She secured Post-Doctoral Medical Fellowship in Pediatric Pulmonology at the Children’s Hospital Los Angeles, Keck School of Medicine at the University of Southern California.
Clinical research has always been a passion for the newly appointed Deputy Director-General for Programmes at the World Health Organisation (WHO) until the time Dr Soumya Swaminathan got into Indian Council of Medical Research (ICMR), an institution of repute as its Director.
Swaminathan’s recent elevation to the post of DDG at WHO is not only a matter of pride for India but will also go a long way in building a credibility for India where she herself has been tirelessly involved in research for diseases like HIV and TB and has been a keen observer of the public health system and different aspects of health programmes in the country.
Most recently, she has been working as Secretary, Department of Health Research – Ministry of Health and Family Welfare, Government of India, and Director General of Indian Council of Medical Research the apex body in India for the formulation, coordination and promotion of Biomedical research.
She credits most of her experience in research and offers her gratitude to the Centre to offer a demanding position to an academician. She opines that her elevation signifies the importance of science, data and evidence as being central to policymaking, medical research and public health. In an interview with Healthy India Chronicle, Dr Swaminathan talks about several key research initiatives and the way forward.
What are the most serious healthcare challenges facing India today and what can be done to tackle them?
Providing quality and affordable healthcare for all in a populous country like India is a challenging task. Large scale development, rapid urbanization, increased mobility of the population, changing climatic conditions are seriously impacting various disease conditions. The emergence and re-emergence of new infections, growing problem of antimicrobial resistance, health inequity, and the increasing burden of non-communicable diseases is a cause for concern. India is still struggling with high incidence of infectious diseases and some pockets are still prone to such infections. Due to epidemiological transition, changing life style and environmental changes the burden of chronic diseases is also becoming more apparent. This is further amplified by multiple risk factors, which continue to create health issues, be it malnutrition, indoor and outdoor air pollution, alcohol, tobacco use, smoking, changed food habits and indulgence on high fat foods are all contributing.
Given the rise in the absolute number of non-communicable diseases, India needs to adopt a multi-pronged, multi-sectoral approach to manage its high disease burden. Air pollution is a major determinant of non-communicable diseases. To effectively deal with this problem, other ministries such as environment and urban development etc. need to be involved. To handle the excess fat, sugar and salt quantities in foods, we need to work on food labelling and increase food taxes. This will need engagement with finance ministry and other sectors.
Strengthening the primary healthcare system and adopting preventive healthcare measures are also very important. Further, given the wide variations in the burden of diseases, it is necessary to generate evidence to build our understanding of the specific disease burden in each state, over and above the useful understanding provided by trends that are common for groups of states at similar levels of epidemiological transition. If the biggest health problems and risks in each state are tackled on priority, the chances of achieving the overall health targets set by India as per the National Health Policy would be much higher than with adopting a more generic approach. The strategy for health action must be aligned to the specific context of each state.
Q: Tell us about ICMR’s vision for research?
The Indian Council of Medical Research has been at the forefront of medical research in the country and has supported national health programmes. We are at a crucial juncture when the world has moved from Millennium Development Goals (MDGs) to Sustainable Development Goals (SDGs).
The Government of India has released the National Health Policy 2017 aiming for universal health coverage. ‘Vision for a Healthy India,’ a document prepared by NITI Aayog provides guidance to health planners and implementers on future strategies and action plan to improve health indicators in the country. The Government of India has also strengthened efforts towards elimination of diseases like leprosy, filariasis, leishmaniasis, tuberculosis and malaria.
ICMR is aligning its research priorities to become truly complementary to national policies. There will be a focus on translating the leads emerging from research to action for the benefit of society and introduction of affordable indigenously developed technologies for disease diagnosis, prevention, treatment and control. The ICMR Strategic Plan & Agenda 2030 provides a roadmap in terms of strategies planned and timelines mentioning the short, medium and long-term goals to be achieved by 2030. ICMR aims to strengthen health research capacity and infrastructure in the country with a special emphasis on developing online and customized courses, infrastructural and mentorship support, and creating centres of excellence as regional hubs for action oriented research. Data management is very crucial for policy making hence, ICMR has proposed to implement an ICMR Policy for sharing and access of data, set up disease specific repositories and research warehouse for improving research and public health as well as carrying out big data analytics. This will help in exploration and generation of new ideas. Through a networkof centres, ICMR will develop research collaborations with AYUSH agencies with a focus on scientific validation of traditional remedies. In addition, ICMR will focus on evidence to policy translation and strengthening of ongoing national health programmes.
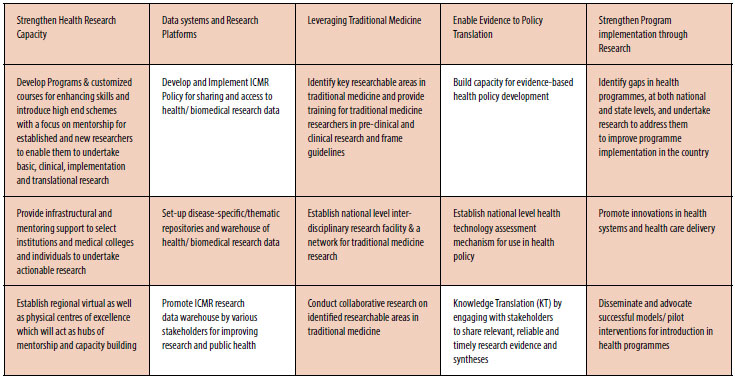
The ICMR Strategic Plan and Agenda 2030 is based on five major pillars of capacity building, data management, leveraging traditional medicine, evidence to policy and strengthening program implementation through research. The ICMR Strategic Plan was supported by a comprehensive research performance evaluation by external agencies. The recommendations of various committees that have reviewed ICMR’s work, recent WHO guidance on elimination of diseases and sustainable development goals and a plan to leverage the strength of ICMR institutional network in India form the foundation on which pillars of ISP-2017 have been built. Its core aim is to deal with health challenges faced by the country such as non-communicable diseases, anti-microbial resistance, emerging infections, maternal and child health and issues related to health systems and health care delivery.
With implementation of ISP 2017, ICMR intends to play a greater role in improving the health of the people of India. As a knowledge generating body, it will position itself to provide critical feeds for policy making and program strengthening and improvement.
The renewed focus on innovation and translation of research into products and schemes of mass benefit is expected to touch the lives of the people of India. I hope that in the years to come, India will emerge as a global leader in health research.
Strategic Framework: 5 Pillars with 15 Goals
How has your experience of working in India equipped you for the new role at the WHO?
I have seen the health system at very close quarters in India. Having worked on a disease like tuberculosis, I have observed the health systems and the social determinants of the disease, both of which are equally important in tackling TB. My experience of working in India has helped me adopt a pragmatic and practical approach of developing strategies that are forward looking as well as designed to for effective implementation on the ground and within the prevalent ecosystem. A lot of work at the WHO involves setting standards and guidelines for countries to follow. My experience will bring in a perspective from the country level with the knowledge of how health systems work in specific political, socio-economic and cultural contexts in developing countries. It is important to draw guidelines that could be followed, has buy-in from all stakeholders, and that will remain one of my key priorities.
























